4 Dec 2019
Think replacement body parts, and The Six Million Dollar Man and The Bionic Woman of 1970s television might spring to mind. But while permanently attached, fully functioning, replacement limbs remain in the future, engineers are behind the replacement of complex joints, attractive artificial limbs and other advances helping build better – and longer – lives.
New Zealand is emerging as a leader in prosthetic implants thanks to biomedical engineering – the combination of engineering, medicine and biology to improve human life. Additive manufacturing (AM), also known as 3D printing, is often key.
Christchurch-based tech firm Ossis was an early adopter of AM more than a decade ago, and uses it to manufacture custom orthopaedic implants in titanium alloy.
As well as being biocompatible and chemically stable in the human body, titanium has good mechanical properties. For example, the titanium screws used to secure the implant into bone comfortably withstand the torque. But titanium’s greatest advantage is that the bone grows onto and adheres to the implant, adding stability, so it has replaced stainless steel implants as the current “go to” choice of implant material.
Ossis Development Engineer, Bethany Oates, says the company has developed porous, open mesh titanium implants through which bone and soft tissue can grow to keep the implant in place. The use of titanium was a breakthrough, she says, because the body accepts it easily.
“For the soft tissues, that’s very important.”

3D-printed prosthetics for the lower arm, the foot and below the knee. Image: Olaf Diegel
Bethany says a 19-year-old woman recently received a titanium implant after a large section of her pelvis was removed due to a tumour. Ossis created a custom-fit titanium implant to replace the missing section, aimed at ensuring the woman will enjoy a comfortable, active life. The intention is for the implant to outlive its host.
To create a custom fit, Ossis uses CT scans to generate a computer model of the patient’s anatomy in the target area. The AM software slices the 3D computer model into thin, two-dimensional digital layers and converts them into machine language for the 3D printer, which creates the physical, three-dimensional object, layer by layer – in this case, in powdered titanium alloy. There is minimal waste as the unused powder is collected and used to grow the next implant. A multi-axis milling machine completes the finishing touches.
“When we first started,” says Bethany, “it was pretty limited, including in the materials you could use, but now they can use titanium and they’re working on carbon.”
This will enable composite implants with specific properties in different layers, or soft and hard areas in the same implant.
It’s all about the optics
Professor Olaf Diegel, head of the Creative Design and Additive Manufacturing Laboratory at the University of Auckland’s Faculty of Engineering, has worked extensively to develop prosthetic limbs in New Zealand and Europe. He says New Zealand’s prosthetics industry has a high number of young people compared with overseas organisations, which are usually staffed by traditional craftspeople.
A key ingredient in biomedical engineering is the ability for experts in different fields to work together.
Surgeons, biologists, software engineers and engineers from other disciplines are all involved in the creation of 3D artificial limbs.
His own team is working with the University’s Ophthalmology Department, developing 3D-printed corneal replacements in collagen-based materials made from fish scales. The engineers are driving the technology but they need the ophthalmologists’ input to ensure the material is suitable for optic engineering. The corneal replacements have a low risk of rejection because human bodies already contain collagen.
Sometimes prosthetics are rejected on emotional grounds, including aesthetics and comfort.
“An amputee’s residual limb gets bigger or smaller depending on their activity through the day, which means standard prosthetics become uncomfortable as the fit changes,” says Olaf.
“We’ve had two students spin out a little company called ProstheteX. They’re doing very light, comfortable prosthetics that expand or contract with the amputee’s limbs.”
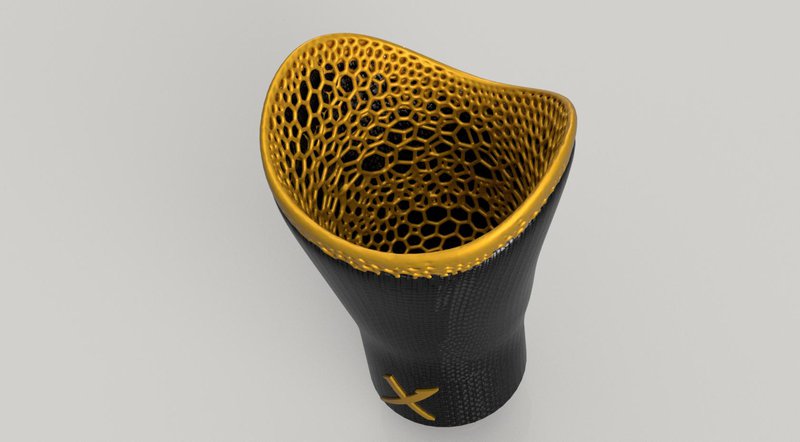
ProstheteX compliant prosthetic socket allows a patient's limb to expand or contract. Image: Sebastian Weaver/Connor Talbot
So far, so good, but with the use of stem cells to create artificial organs, it gets controversial. Simple organs such as bladders and tracheas are created overseas using layers of the patient’s stem cells suspended in hydrogel. The stem cells “know” they’re supposed to be a bladder so they grow into the bladder and replace the hydrogel. The risk of rejection is small.
The next step, to complex organs, is still two or three decades away. A new pancreas would cure diabetes overnight; a new kidney would free a patient from dialysis, but these complex organs are dependent on artificial vascular systems.
“Once they crack that, they’ll be able to print the more complex organs,” Olaf says.
“I’m pretty confident that in my lifetime it will happen.”
It raises questions around whether such expensive treatment will be widely available and how long humans want to live.
Breathe easy
Fisher & Paykel Healthcare is also developing new materials to make treatment more comfortable for patients. The company designs and manufactures humidification products for use in respiratory care, acute care, surgery and the treatment of obstructive sleep apnea.
With a degree in mechanical engineering, an MBA and substantial experience in the medical device industry, Laurence Gulliver is the company’s General Manager – Noninvasive Ventilation. He oversees the team that designs masks and tubes to deliver optimum humidity levels while a patient is being ventilated in hospital. Humidity helps ensure the respiratory system isn’t damaged by dry gas going into the lungs.
“With noninvasive ventilation, two of the biggest challenges are patient discomfort and condensation in the tubes that deliver the treatment,” says Laurence.
We use innovative materials like silicone to make masks that are softer and more flexible and can adjust to different face shapes.
“To improve comfort, we developed a technology called Rollfit using silicone, which helps minimise pressure on the nasal bridge while maintaining a secure seal over the nose.”

Laurence Gulliver with Fisher & Paykel Healthcare's Rollfit technology. Image: Fisher & Paykel Healthcare
When a patient is being ventilated, drops of water can build up in the delivery tubes, interfering with the patient’s breathing. Opening the breathing circuit to remove the condensation can expose the patient to bacteria or infection.
“We solve this problem by developing clever surface finishes and permeable materials that ‘breathe’,” says Laurence.
“This allows water vapour to diffuse right through the tubing wall.”
This article was originally published in the December 2019 issue of EG magazine.